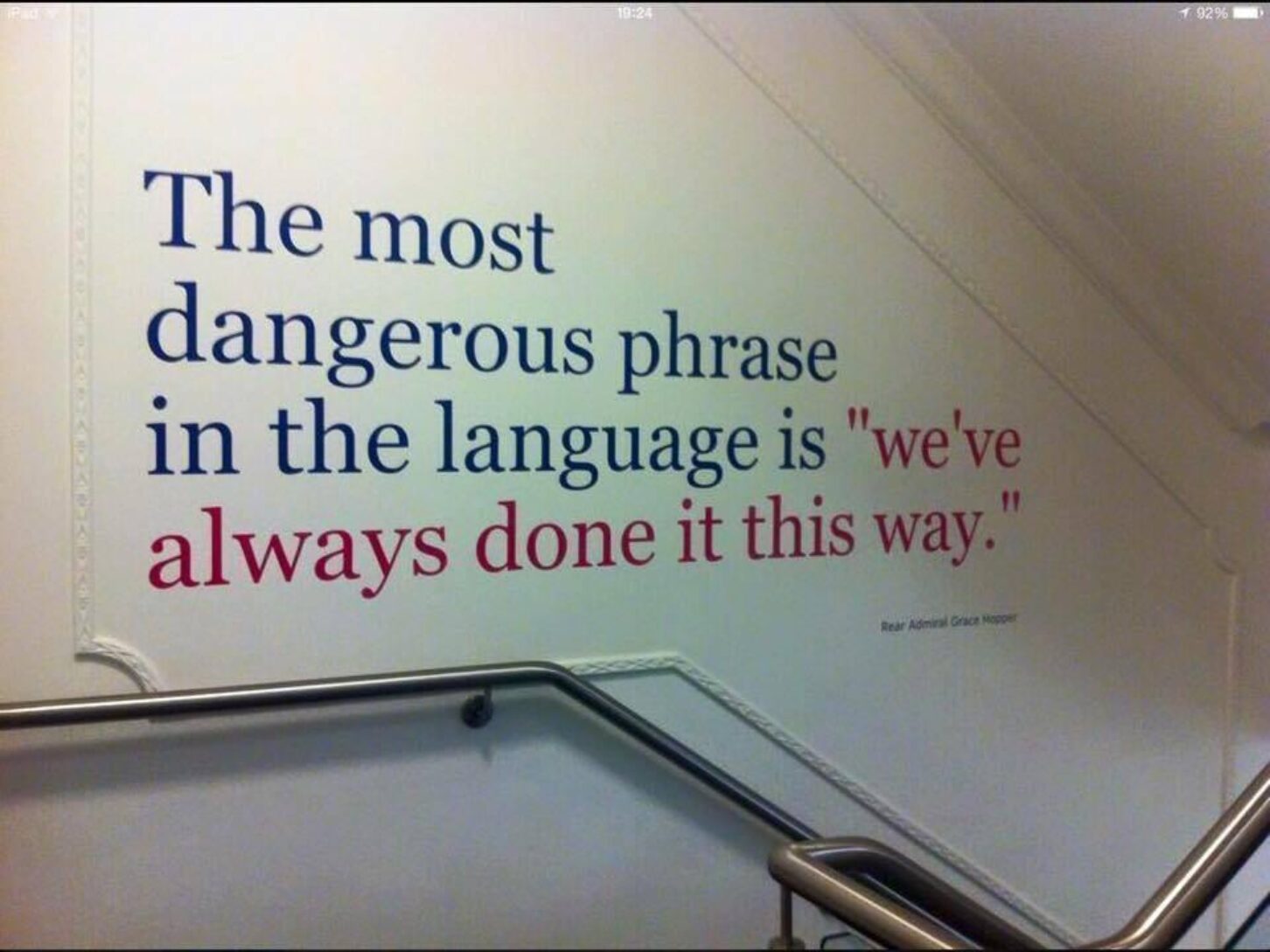
Telemedicine, Healthcare.gov and the danger of “we’ve always done it this way.”
Health Policy News and Views
Compiled by Benita M. Dodd

I shared a recollection on Facebook recently that is simply amazing in its lesson that it can be a deadly mistake to accept that, “That’s the way we’ve always done it.”
I was visiting the Friendly Human studios down at Atlanta’s Tech Village a couple of years ago, and got into a discussion with one of the company execs. We were talking about innovation in doing things, etc.
He shared his experience at a medical convention he’d gone to videotape and the story he heard from an oncologist panelist. (It’s been a while and I’m paraphrasing big-time, so bear with me.)
The oncologist said he’d been treating brain cancer patients, and the rule was you could only treat three brain lesions with radiology at one sitting.
He started wondering what was the thinking behind treating only three lesions. Was it because any more lesions than three meant it was a hopeless case? Were you terminal? Could the ailing patient not tolerate any more than that?
 He decided to research the reason behind it. Finally after months of research, he tracked down the author of the original protocol and called him up to ask him why three lesions was the magic number all these years.
He decided to research the reason behind it. Finally after months of research, he tracked down the author of the original protocol and called him up to ask him why three lesions was the magic number all these years.
“It took so long to treat patients with the equipment we had,” the man replied. “The only way we could treat more patients with our limited resources was to limit the use of the equipment.”
Consider how many people had been sentenced to death in the interim, even as the technology and equipment advanced … All because nobody bothered to stop and ask, “Why?”
The story stuck with me, but it took a long time to remember who told it to me. When I finally tracked down Daniel Roberts of Friendly Human and got him to confirm he was the source, he named the surgeon: Dr. Robert Hesselgesser at the LGK Society (Leksell Gamma Knife Society) conference in New York City. “Amazing guy,” Roberts declared. “He was brilliant, but also brilliant at explaining it.” That’s the kind of physician I want on my side.
‘Faceplants’: An article that shared some graphic before and after photographs of full-face transplants got me thinking. Not long ago, if you were a burn, accident or crime victim with deforming facial injuries, you had no option but to live with it and endure the horrified stares. Today, surgeons are transplanting entire faces from deceased people onto such patients. Pretty soon, though, I suspect researchers will find a way to grow skin from the patient’s own cells, sculpt a “face” on a mold and place that new face on such patients. Technology and innovation are advancing at incredible speed; some labs are already growing “sheets” of skin!
The warning signs were there: During the two years before the disastrous opening of HealthCare.gov, federal officials in charge of creating the online insurance marketplace received 18 written warnings that the mammoth project was mismanaged and off course but never considered postponing its launch, according to government investigators. The Washington Post details the findings from an exhaustive two-year inquiry by HHS’s Office of Inspector General into the failings of HealthCare.gov, which crashed within two hours of its launch on Oct. 1, 2013.
Health care stasis: “Direct care” legislation is stalled in the Georgia Senate as Crossover Day approaches unless sponsors can attach it to a House bill. It’s disappointing to think Georgians could miss out on this affordable, effective health care option. Read the Foundation’s recent commentary here; read the Heritage Foundation study on direct care here. As I noted in my last post, because direct care doesn’t cover specialists or emergencies, consumers still need a high-deductible health plan, but you get lower-cost coverage by combining the health plan premiums and the monthly direct primary care fee. The legislation would ensure that the option – which works much like a fitness club or AAA membership – is not considered insurance.
Under the Gold Dome: The Georgia Right To Try Act bill passed unanimously out of the state House. Still alive is scope-of practice expansion legislation that would enable dental hygienists to administer local anesthesia under direct supervision of a dentist. Forty-four states and the District of Columbia allow this already. Can you say “protectionist”?
Saving money and patients: Not only is telemedicine a money-saver, but research shows it delivers better quality care than in-person, writes Sally C. Pipes of the Pacific Research Institute in the Tampa Tribune. She cites a University of Massachusetts Medical School study of 110,000 Intensive-care patients. Some received medical attention from remote specialists with basic monitoring from on-site doctors. Others received traditional in-hospital care. Patients with access to telehealth services were 26 percent more likely to survive the ICU and were discharged from the unit 20 percent faster than those without telehealth access.
Transparency: Knowing the cost of procedures is crucial to decision-making in consumer-driven health care. A Web site by nonprofit FAIR Health helps consumers estimate medical and dental expenditures. Consumers enter a location, whether they are insured and the type of service or procedure. They can then view a specific medical code, the estimated cost for that service or procedure, estimated reimbursement and out-of-pocket cost. Reporting on the service, WPVI notes that estimates on facility fees are expected to be added in the next couple months. FAIR Health also offers an app.
Quote of Note
George Orwell said, ‘If people cannot write well, they cannot think well, and if they cannot think well, others will do their thinking for them.’ If Orwell was right, the profession of medicine and the patients it cares for could be in big trouble. As a result of ongoing changes in health care, today’s medical students and residents are being asked to write much less than in the past, with a predictable decline in the quality of what they produce. This, in turn, threatens the quality of patient care.” – Richard Gunderman and James Lynch
Health Policy News and Views
Compiled by Benita M. Dodd

BENITA DODD
I shared a recollection on Facebook recently that is simply amazing in its lesson that it can be a deadly mistake to accept that, “That’s the way we’ve always done it.”
I was visiting the Friendly Human studios down at Atlanta’s Tech Village a couple of years ago, and got into a discussion with one of the company execs. We were talking about innovation in doing things, etc.
He shared his experience at a medical convention he’d gone to videotape and the story he heard from an oncologist panelist. (It’s been a while and I’m paraphrasing big-time, so bear with me.)
The oncologist said he’d been treating brain cancer patients, and the rule was you could only treat three brain lesions with radiology at one sitting.
He started wondering what was the thinking behind treating only three lesions. Was it because any more lesions than three meant it was a hopeless case? Were you terminal? Could the ailing patient not tolerate any more than that?
 He decided to research the reason behind it. Finally after months of research, he tracked down the author of the original protocol and called him up to ask him why three lesions was the magic number all these years.
He decided to research the reason behind it. Finally after months of research, he tracked down the author of the original protocol and called him up to ask him why three lesions was the magic number all these years.
“It took so long to treat patients with the equipment we had,” the man replied. “The only way we could treat more patients with our limited resources was to limit the use of the equipment.”
Consider how many people had been sentenced to death in the interim, even as the technology and equipment advanced … All because nobody bothered to stop and ask, “Why?”
The story stuck with me, but it took a long time to remember who told it to me. When I finally tracked down Daniel Roberts of Friendly Human and got him to confirm he was the source, he named the surgeon: Dr. Robert Hesselgesser at the LGK Society (Leksell Gamma Knife Society) conference in New York City. “Amazing guy,” Roberts declared. “He was brilliant, but also brilliant at explaining it.” That’s the kind of physician I want on my side.
‘Faceplants’: An article that shared some graphic before and after photographs of full-face transplants got me thinking. Not long ago, if you were a burn, accident or crime victim with deforming facial injuries, you had no option but to live with it and endure the horrified stares. Today, surgeons are transplanting entire faces from deceased people onto such patients. Pretty soon, though, I suspect researchers will find a way to grow skin from the patient’s own cells, sculpt a “face” on a mold and place that new face on such patients. Technology and innovation are advancing at incredible speed; some labs are already growing “sheets” of skin!
The warning signs were there: During the two years before the disastrous opening of HealthCare.gov, federal officials in charge of creating the online insurance marketplace received 18 written warnings that the mammoth project was mismanaged and off course but never considered postponing its launch, according to government investigators. The Washington Post details the findings from an exhaustive two-year inquiry by HHS’s Office of Inspector General into the failings of HealthCare.gov, which crashed within two hours of its launch on Oct. 1, 2013.
Health care stasis: “Direct care” legislation is stalled in the Georgia Senate as Crossover Day approaches unless sponsors can attach it to a House bill. It’s disappointing to think Georgians could miss out on this affordable, effective health care option. Read the Foundation’s recent commentary here; read the Heritage Foundation study on direct care here. As I noted in my last post, because direct care doesn’t cover specialists or emergencies, consumers still need a high-deductible health plan, but you get lower-cost coverage by combining the health plan premiums and the monthly direct primary care fee. The legislation would ensure that the option – which works much like a fitness club or AAA membership – is not considered insurance.
Under the Gold Dome: The Georgia Right To Try Act bill passed unanimously out of the state House. Still alive is scope-of practice expansion legislation that would enable dental hygienists to administer local anesthesia under direct supervision of a dentist. Forty-four states and the District of Columbia allow this already. Can you say “protectionist”?
Saving money and patients: Not only is telemedicine a money-saver, but research shows it delivers better quality care than in-person, writes Sally C. Pipes of the Pacific Research Institute in the Tampa Tribune. She cites a University of Massachusetts Medical School study of 110,000 Intensive-care patients. Some received medical attention from remote specialists with basic monitoring from on-site doctors. Others received traditional in-hospital care. Patients with access to telehealth services were 26 percent more likely to survive the ICU and were discharged from the unit 20 percent faster than those without telehealth access.
Transparency: Knowing the cost of procedures is crucial to decision-making in consumer-driven health care. A Web site by nonprofit FAIR Health helps consumers estimate medical and dental expenditures. Consumers enter a location, whether they are insured and the type of service or procedure. They can then view a specific medical code, the estimated cost for that service or procedure, estimated reimbursement and out-of-pocket cost. Reporting on the service, WPVI notes that estimates on facility fees are expected to be added in the next couple months. FAIR Health also offers an app.
Quote of Note
George Orwell said, ‘If people cannot write well, they cannot think well, and if they cannot think well, others will do their thinking for them.’ If Orwell was right, the profession of medicine and the patients it cares for could be in big trouble. As a result of ongoing changes in health care, today’s medical students and residents are being asked to write much less than in the past, with a predictable decline in the quality of what they produce. This, in turn, threatens the quality of patient care.” – Richard Gunderman and James Lynch
Benita Dodd is vice president of the Georgia Public Policy Foundation.
